Thank you for attending the NAADAC Webinar, Supporting Those Who Served: Substance Abuse and Comprehensive Mental Health for Military Affiliated Populations
For more information regarding the Comprehensive Veteran Mental Health Model, see below
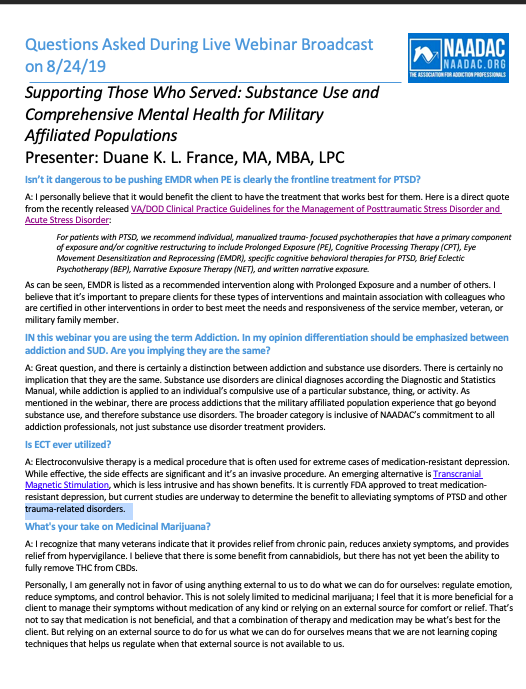
Questions Asked During the Live Webinar Broadcast
Further Reading and Listening
www.veteranmentalhealth.com/ptsd/
www.veteranmentalhealth.com/tbi/
www.veteranmentalhealth.com/emotion/
www.veteranmentalhealth.com/substance-abuse/
www.veteranmentalhealth.com/purpose-meaning/
www.veteranmentalhealth.com/moral-injury/
www.veteranmentalhealth.com/needs/
www.veteranmentalhealth.com/family/
REFERENCES
Brenner, L. A., Homaifar, B. Y., Adler, L. E., Wolfman, J. H., & Kemp, J. (2009). Suicidality and veterans with a history of traumatic brain injury: Precipitating events, protective factors, and prevention strategies. Rehabilitation Psychology, 54(4), 390.
Carmona-Perera, M., Verdejo-García, A., Young, L., Molina-Fernández, A., & Pérez-García, M. (2012). Moral decision-making in polysubstance dependent individuals. Drug and alcohol dependence, 126(3), 389-392.
Glasner-Edwards, S., & Rawson, R. (2010). Evidence-based practices in addiction treatment: Review and recommendations for public policy. Health policy, 97(2-3), 93-104.
Hall, L. K. (2016). Counseling military families: What mental health professionals need to know. Routledge.
Henkel, D. (2011). Unemployment and substance use: a review of the literature (1990-2010). Current drug abuse reviews, 4(1), 4-27.
Karlin, B. E., Ruzek, J. I., Chard, K. M., Eftekhari, A., Monson, C. M., Hembree, E. A., … & Foa, E. B. (2010). Dissemination of evidence‐based psychological treatments for posttraumatic stress disorder in the Veterans Health Administration. Journal of traumatic stress, 23(6), 663-673.
Keshen, A. (2006). A new look at existential psychotherapy. American Journal of Psychotherapy, 60(3), 285-298.
Hellmuth, J. C., Stappenbeck, C. A., Hoerster, K. D., & Jakupcak, M. (2012). Modeling PTSD symptom clusters, alcohol misuse, anger, and depression as they relate to aggression and suicidality in returning US veterans. Journal of traumatic stress, 25(5), 527-534.
Kulka, R. A. (1990). The national Vietnam veterans readjustment study: Tables of findings and technical appendices. Brunner/Mazel Publisher.
Litz, B. T., Stein, N., Delaney, E., Lebowitz, L., Nash, W. P., Silva, C., & Maguen, S. (2009). Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical psychology review, 29(8), 695-706.
Padgett, D. K., Henwood, B., Abrams, C., & Drake, R. E. (2008). Social relationships among persons who have experienced serious mental illness, substance abuse, and homelessness: Implications for recovery. American journal of orthopsychiatry, 78(3), 333-339.
Paley, B., Lester, P., & Mogil, C. (2013). Family systems and ecological perspectives on the impact of deployment on military families. Clinical child and family psychology review, 16(3), 245-265.
Scholten, J., Vasterling, J. J., & Grimes, J. B. (2017). Traumatic brain injury clinical practice guidelines and best practices from the VA state of the art conference. Brain injury, 31(9), 1246-1251.
Schuman, D. (2016). Veterans’ experiences using complementary and alternative medicine for posttraumatic stress: A qualitative interpretive meta-synthesis. Social work in public health, 31(2), 83-97.
Southwick, S. M., Gilmartin, R., Mcdonough, P., & Morrissey, P. (2006). Logotherapy as an adjunctive treatment for chronic combat-related PTSD: A meaning-based intervention. American Journal of Psychotherapy, 60(2), 161.
Stappenbeck, C. A., Hellmuth, J. C., Simpson, T., & Jakupcak, M. (2014). The effects of alcohol problems, PTSD, and combat exposure on nonphysical and physical aggression among Iraq and Afghanistan war veterans. Psychological Trauma: Theory, Research, Practice, and Policy, 6(1), 65.
Walton, J. L., Raines, A. M., Cuccurullo, L. A. J., Vidaurri, D. N., Villarosa‐Hurlocker, M. C., & Franklin, C. L. (2018). The relationship between DSM‐5 PTSD symptom clusters and alcohol misuse among military veterans. The American journal on addictions, 27(1), 23-28.
Weiss, N. H., Williams, D. C., & Connolly, K. M. (2015). A preliminary examination of negative affect, emotion dysregulation, and risky behaviors among military veterans in residential substance abuse treatment. Military behavioral health, 3(4), 212-218.
Wenzel, S. L., Bakhtiar, L., Caskey, N. H., Hardie, E., Redford, C., Sadler, N., & Gelberg, L. (1995). Homeless veterans’ utilization of medical, psychiatric, and substance abuse services. Medical Care.
Do you want to learn more about Veteran Mental Health? Check out the two Head Space and Timing Books
▬▬▬▬▬▬▬ SUBSCRIBE ▬▬▬▬▬▬▬
Click Here to Subscribe to the Head Space and Timing Blog!
▬▬▬▬▬▬▬ STAY CONNECTED WITH DUANE▬▬▬▬▬▬▬
*** Use & search hashtag: #VeteranMentalHealth ***
Email Address → duane@veteranmentalhealth.com